Mips Quality Measures Diabetes

Select at least 1 outcome measure.
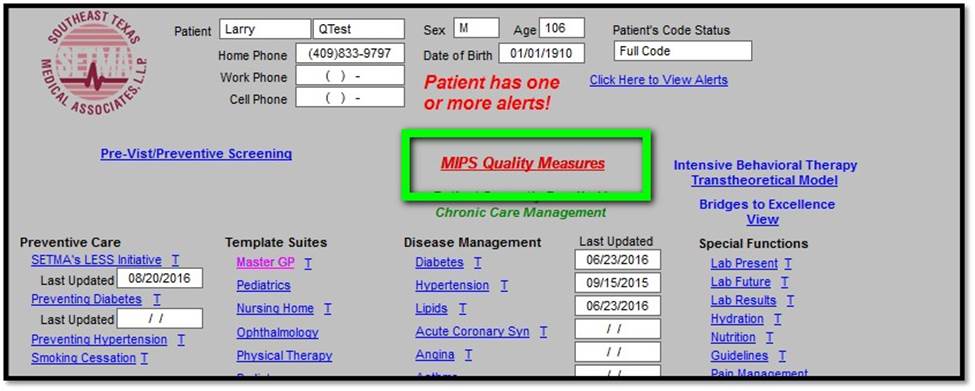
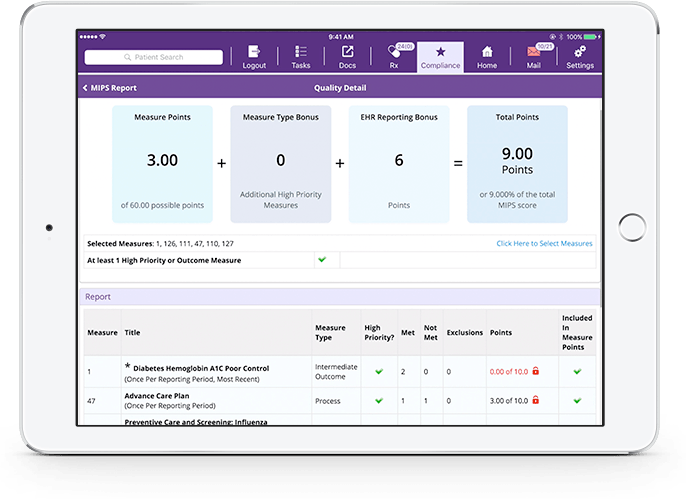
Mips quality measures diabetes. Mips clinical quality measures cqms measure type. Measure data may be submitted by individual mips eligible clinicians groups or third party intermediaries. This measure is to be submitted a minimum of once per performance period for patients with diabetes seen during. There are 6 collection types for quality measures.
What is a flat. Merit based incentive payment system mips quality measure data. If no outcome measures are applicable to your patient population then you must select at least one. Mips quality performance category.
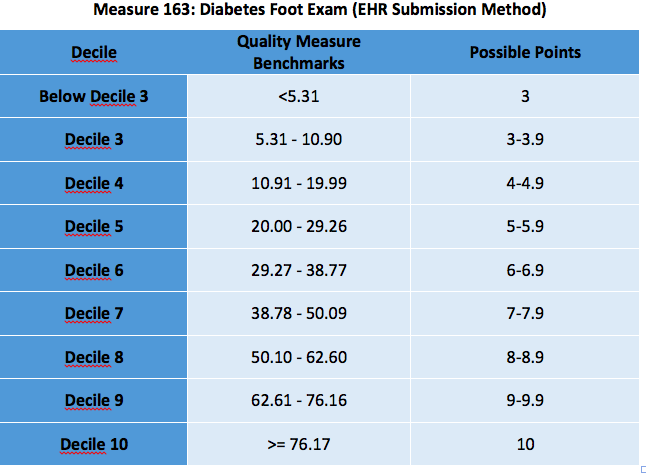
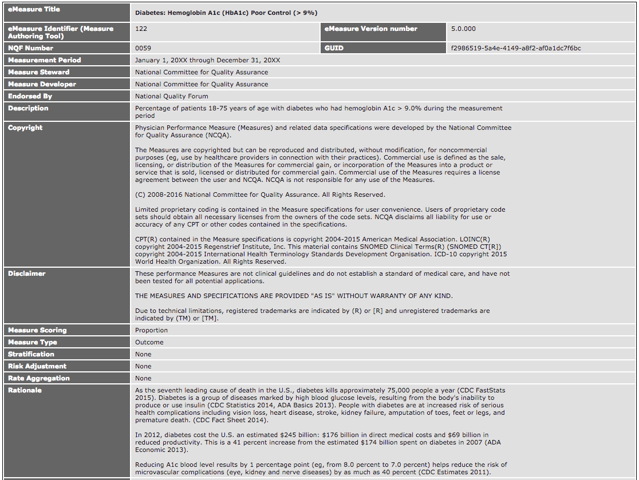
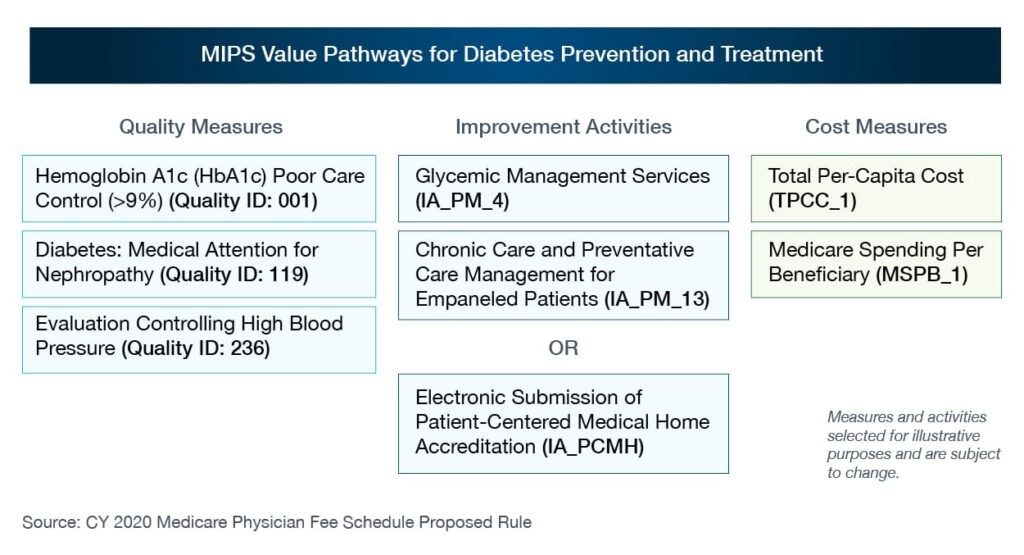
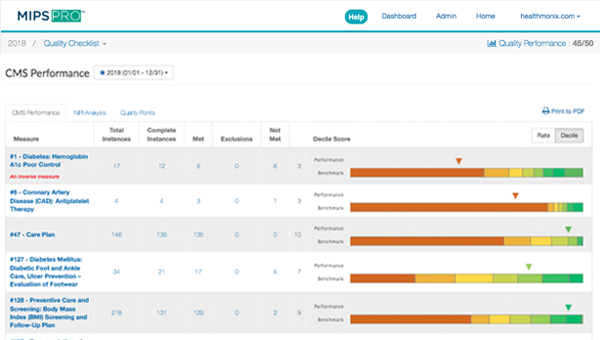
For the mips quality performance category you must report at least one outcome measure. Auditors are provided with high level supporting documentation guidelines that are based upon the mips quality measures specification documents. The most recent quality data code submitted will be used. Hemoglobin a1c poor control 9 what is the 7 point cap.
Quality cost improvement. Percentage of patients 18 75 years of age with diabetes who had hemoglobin a1c 9 0 during the measurement period instructions. Intermediate outcome high priority description. Once a quality measure is in its second year of being topped out you won t be able to score more than 7 achievement points for it.
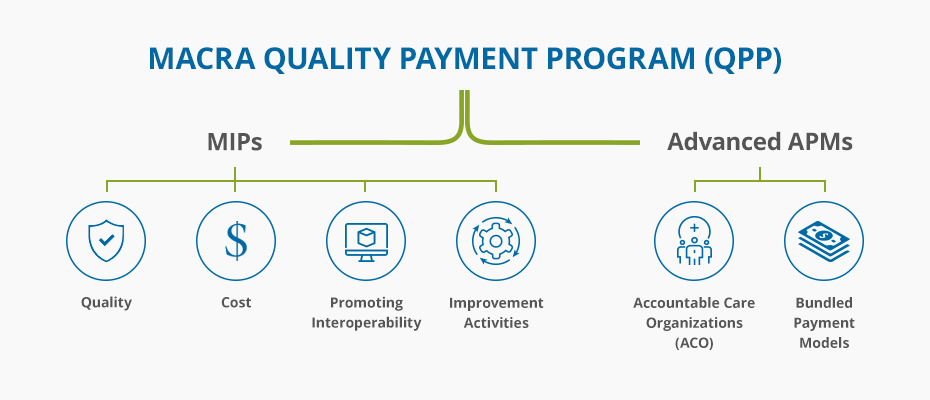
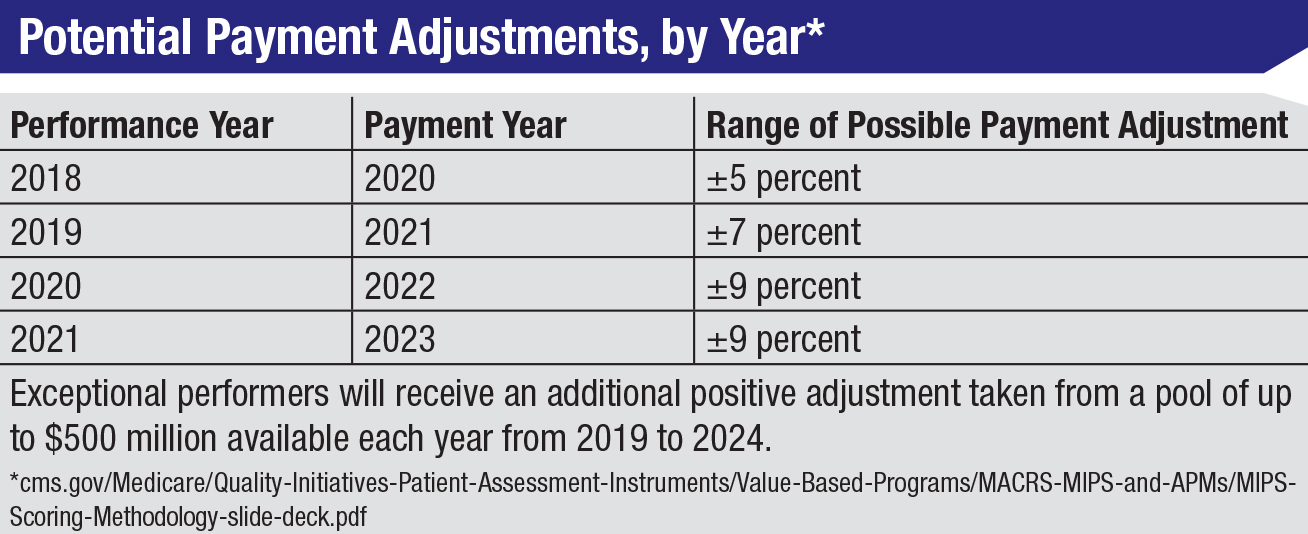
Percentage of patients 18 75 years of age with diabetes who had hemoglobin a1c 9 0 during the measurement period instructions. This measure may be submitted by merit based incentive payment system mips eligible clinicians who perform the quality actions described in the measure based on services provided and the measure. An inverse quality measure is one where you earn more achievement points for a lower performance rate. Merit based incentive payment system mips mips is part of cms s quality payment program and was designed to tie payments to quality and cost efficient care drive improvement in care processes and health outcomes increase the use of healthcare information and reduce the cost of care.
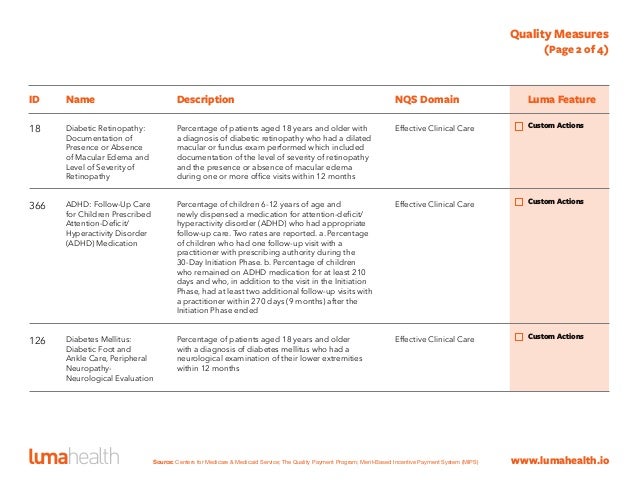
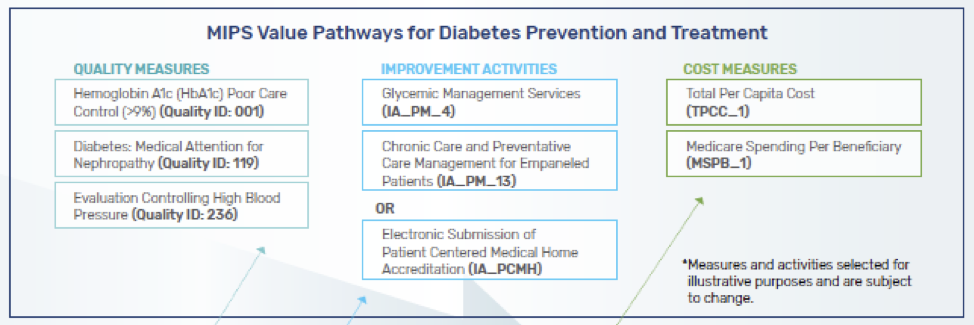
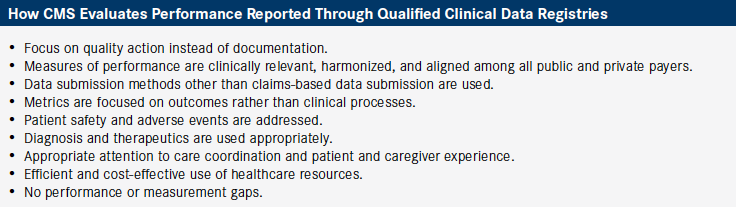
Electronic clinical quality measures ecqms mips clinical quality measures cqms qualified clinical data registry qcdr measures. Diabetes endocrinology mips quality measures and improvement activities how to select mips quality measures step 1. This measure is to be submitted a minimum of once per performance period for patients with diabetes seen during the performance period. The merit based incentive payment system mips track of medicare s quality payment program qpp includes four performance categories.
You must collect measure data for the 12 month performance period january 1 december 31 2020. The numerator options included in this specification are used to submit the quality actions as allowed by the measure. This measure is to be submitted a minimum of once per performance period for patients with diabetes mellitus seen during the performance period. Meeting quality measures through diabetes self.