Mips Quality Measures For Anesthesia
The 2020 quality payment program qpp final rule was published on november 15 2019 and we have 5 key highlights and changes that could impact your anesthesia quality reporting.
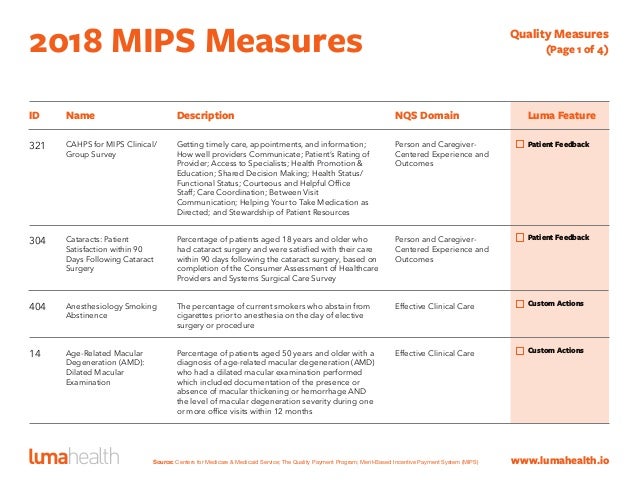
Mips quality measures for anesthesia. Report 6 measures including one outcome or other high priority measure for 12 months on at least 70 of eligible encounters to possibly earn more than 3 points on a measure. Anesthesia providers and groups can select measures from the list of cms approved mips measures at the qpp website. Alternatively they may select to report on quality performance using specialized measures developed by a qualified clinical data registry qcdr of their choosing. Mips measures relevant to anesthesiology quality 70 of total score.
Merit based incentive payment system mips quality measure data. This page provides access to all dermatology specific measures that can be reported for mips. You must collect measure data for the 12 month performance period january 1 december 31 2020. Electronic clinical quality measures ecqms mips clinical quality measures cqms qualified clinical data registry qcdr measures.
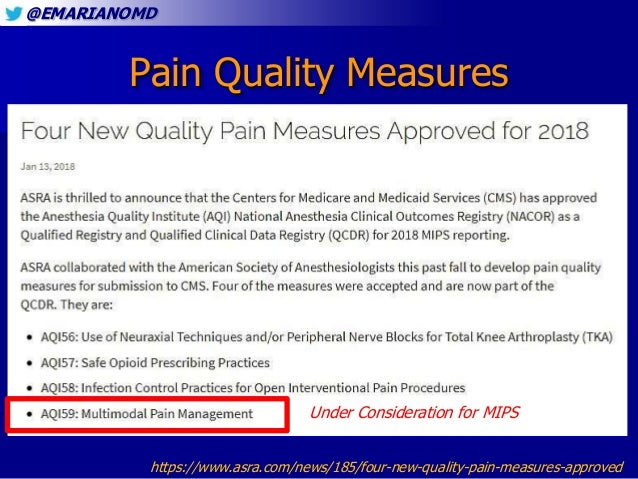
If a measure set has less than 6 measures eligible groups and clinicians must report all measures in the set. This measure may look familiar if you reported mips last year through the asa as it was aqi59. Final measure specification documentation has not been published by cms yet however we would expect this to mirror the aqi measure 59 in which it is. Cms has adopted this measure as a regular mips measure for 2020.
There are 6 collection types for quality measures. For the 2018 mips quality component mips eligible clinicians must report at least six 6 measures for a minimum of 90 days. Approved by the anesthesia quality institute. Select the measure number to download a pdf containing detailed information on measure specifications and requirements.
Learn about 2020 quality measures for mips reporting. If fewer than six 6 measures apply to the eligible clinician the eligible clinician must report on all applicable measures. New mips measure for anesthesia june 3 2020. If no outcome measures are applicable to your patient population then you must select at least one high priority measure see step 2.
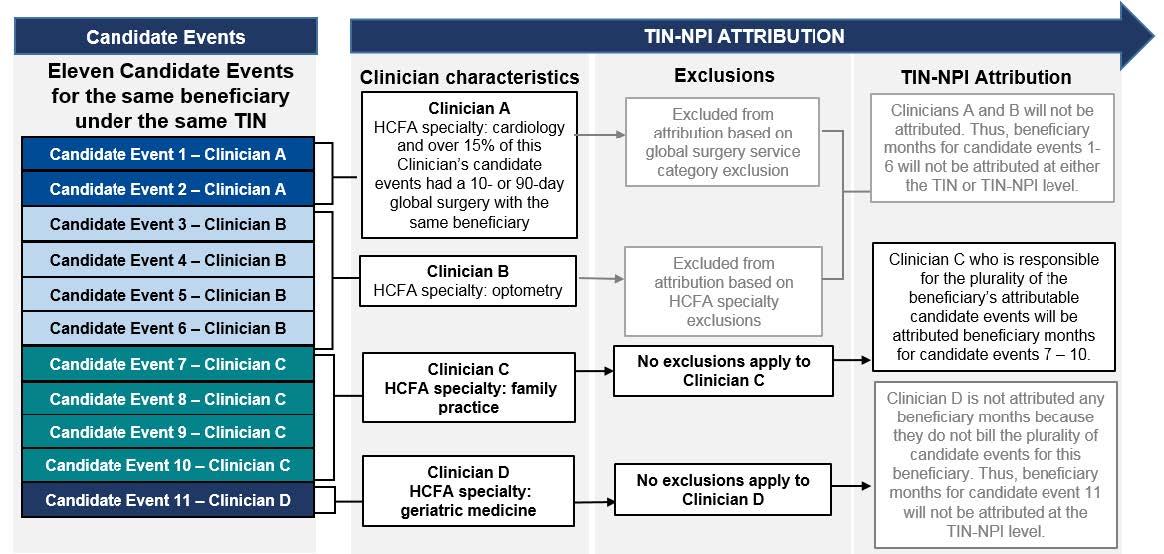
For the mips quality performance category you must report at least one outcome measure. Qcdr measures must be approved each year by cms. Mips eligible clinicians or groups who are reviewing 2019 mips performance feedback and believe there is a discrepancy in the 2019 report can request a targeted review by october 5 2020. This is up from 60 in 2019.
Anesthesiologists may elect to submit quality measures through any of the following mechanisms. Ioh quality measure supports an increasing desire for objective quality measurement and reporting with. The outcome measures you report count towards the six measure requirement for the quality performance category. Measure 477 multimodal pain management.
Anesthesiology mips specialty measure set 2020 cms specialty measure sets may be reported as an alternative to reporting 6 separate quality measures.